Abstract
Many commentators, activists, academics and public health agencies continue to assert or imply that an outbreak of serious and fatal lung injuries that occurred primarily in the United States between mid-2019 and early 2020 may have been caused in part by nicotine vaping. This condition is often known as “EVALI” (E-cigarette, or Vaping, product use-Associated Lung Injury), a term coined by the US Centers For Disease Control and Prevention (CDC). However, an examination of the evidence shows that EVALI cannot have been caused by nicotine vaping. The characteristics of the lung injury outbreak are consistent with localised supply chain contamination. The contaminant has been identified and is known to be Vitamin E Acetate. This had been used a thickener or cutting agent in illicit Tetrahydrocannabinol (THC) cannabis vape pens. This agent cannot be added to nicotine vaping liquids and would serve no useful purpose if it could be. No other or cause or causal agent has been identified that would implicate nicotine liquids and that would be consistent with the geographical and temporal pattern of this lung injury outbreak. There is a vanishing small chance that a second cause would be found in nicotine liquids, coinciding with the same geography, timing and symptoms as Vitamin E Acetate contamination of THC oils. Further, it is highly unlikely that this hypothetical and currently unidentified cause would disappear in early 2020 without some identifiable remedial action in nicotine vaping products. But there has been no identifiable remedial action – nicotine vaping products have not changed, but EVALI has largely gone. The attribution of EVALI to nicotine vaping should stop, the term EVALI should be replaced, risk communicators should shoulder their responsibility to correct residual false risk perceptions, and serious consideration given to the advantages of legalising and regulating cannabis products.
Introduction
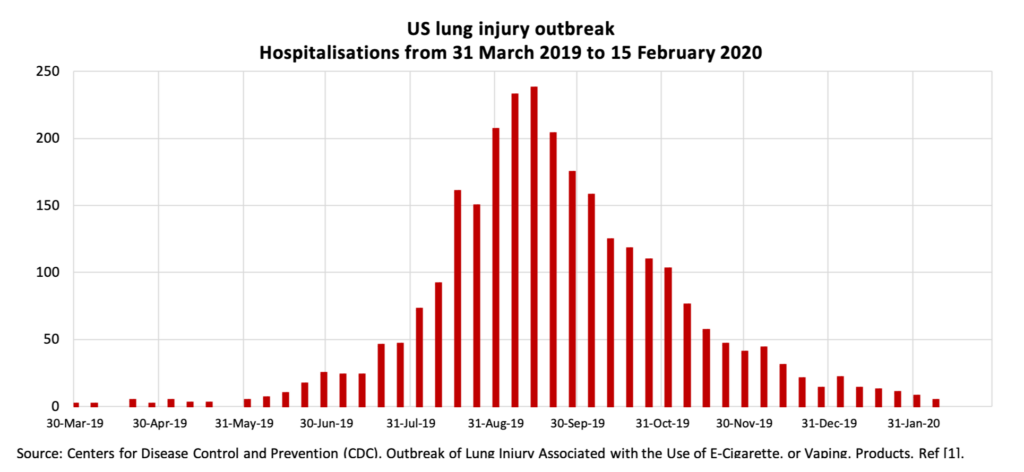
The outbreak of lung injuries in the United States caused the hospitalisation of over 2,800 and the deaths of 68 mostly young people in the period between March 2019 and February 2020 (CDC).[1] The outbreak generated a large volume of commentary and news coverage about vaping, much of it confusing or misleading (Gartner et al. 2020)[2] and prompting political and regulatory overreactions (Hall et al. 2020).[3] The response of public health agencies and the media led to adverse changes in the perceptions of nicotine vaping risk in the United States (Dave et al. 2020)[4]. Though the outbreak was almost entirely US-based, it had an effect on risk perceptions beyond the US. For example, risk perceptions were adversely affected in the UK (Tattan-Birch et al. 2020)[5], where the impact was picked up in ASH(UK) / YouGov surveys as a negative step-change between 2019 and 2020 in smokers’ perceptions of the harms of e-cigarettes.[6]
Analysis: why nicotine vaping is not implicated in EVALI
- The lung disease outbreak was limited in time from mid-2019 to early-2020, peaking in September 2019 and with cases tailing off by February 2020, to the point that CDC stopped reporting on it in February 2020 (CDC hospitalisation data – see the cover image for this paper)[1]. The ‘EVALI” outbreak is essentially over. It did not appear in THC or nicotine vape products at scale before this period and largely disappeared after this period. It was also limited in geography, primarily to North America.[7] This geographic and temporal pattern is consistent with a cause related to localised contaminated supply (comparable to a food poisoning outbreak). It means EVALI cannot be intrinsic to nicotine or THC vaping products because it would have been seen at other times and in other places, given nicotine vaping has been a worldwide phenomenon since around 2010. The U.S. lung injury outbreak must have been caused by something about the products available in North America in the later half of 2019.
- The contaminating agent has been identified. This is Vitamin E Acetate (VEA) (Blount et al. 2020)[8]. Its exact biochemical interaction with lung tissue may be uncertain and is a subject of ongoing work, but there is no real doubt that it played a causal role. It is possible that thickeners with similar chemical or physical properties to VEA could have a role, but none has been identified so far, and attention has focussed exclusively on VEA. CDC has acknowledged this: according to Dr Anne Schuchat, CDC’s principal deputy director in 2019: “we can conclude that what I call the explosive outbreak of cases of EVALI can be attributed to exposure to THC-containing vaping products that also contained Vitamin E acetate” (CDC published transcript, 20 December 2019)[9]
- Vitamin E Acetate was added to illicit THC vapes as a thickener or ‘cutting agent’ to dilute the strength of expensive THC-containing oils while maintaining the viscosity of the liquid. Viscosity is regarded by THC users as a mark of product strength and quality. The addition of VEA to THC vaping oils served an economic purpose, albeit a criminal and disreputable economic purpose. The supply chain involves makers of thickeners and final sellers of illicit THC vape pens. The first signs that thickeners were culpable emerged in August 2019. More information on the companies and products involved is available in the specialist cannabis publication, Leafly.[10][11]
- This agent, VEA, cannot be added to nicotine e-liquids (Kozlovich et al, 2021).[12] It is not soluble in the base liquids, propylene glycol and vegetable glycerin, used for nicotine vaping. Further, it would serve no useful economic purpose even if it could be added. That is because these base liquids are cheap and readily available, and it is simple to dilute any nicotine liquid to a desired strength. Also, there is no reason to add any thickener to a nicotine liquid product because liquid viscosity has no significance for nicotine vapers. For nicotine liquids to be implicated in EVALI, a different cause or causal agent would be required. None has been identified. (See further discussion at point 9 below).
- CDC data shows that the EVALI cases had largely cleared up by early 2020 (see title chart above).[1] This is consistent with the North American illicit supply chain steadily emptying of VEA-contaminated THC products. It would be consistent with remedial action taken to address the risk in VEA-contaminated THC vapes by removing the VEA and using different thickeners or no thickeners. The criminal suppliers have strong incentives not to harm or kill their customers, not to increase their criminal liability, and not to degrade consumer confidence in their products. They will have removed VEA as soon as it became clear this was a causal agent in EVALI, probably starting in August 2019.
- No equivalent remedial action has been taken with nicotine vapes. It is not possible to identify any changes to e-liquid ingredients, devices or manufacturing processes for nicotine vaping products that would have ended their hypothetical role in causing EVALI. Such changes would need to address a speculative cause that remains unknown but is specific to the geography and timing of EVALI. Yet, without any apparent change to nicotine vaping products, EVALI has dwindled to negligible levels. The absence of any remedial actions reinforces the case that nicotine vaping products never had a role in EVALI.
- To recap: for nicotine vaping to be implicated in EVALI, there would need to be a cause other than VEA, yet none has so far been identified. That unknown cause would have to have emerged at the same time, in the same limited geography, and cause the same symptoms as VEA exposure. The unidentified cause would have to have been somehow eliminated in order for the EVALI incidence to decline to trivial levels by February 2020. However, no known remedial action has been taken with nicotine vapes. The chance of all this happening is vanishingly small (i.e. zero), and therefore it is beyond reasonable doubt that it did not happen and nicotine vaping is not implicated in EVALI.
- There is some uncertainty about attributing all the EVALI cases definitively to contaminated THC vapes, but that does not justify extending the uncertainty to nicotine vaping for the reasons described in 1-7 above. The major source of uncertainty is in the sporadic and ad hoc testing of EVALI patients for THC or VEA exposure, and in the poor reliability of users’ accounts of their exposure. It is not at all surprising that some illicit THC users would deny illicit THC use – it could cause them difficulties (real or perceived) with their parents, school, college, employer, parole officer, and/or law enforcement. This point was made by Dr. Scott Aberegg, a critical care pulmonologist at University of Utah Health, in comments to CNBC: “It may turn out there are only two kinds of people who get this disease: those who vape THC and those who won’t admit it”.[13] The epidemiological approach described above is a more reliable way to assess the causes of the lung injury outbreak than user testimony.
- Several theories have been advanced for how nicotine vapes could cause acute lung injury. With reference to Maddison et al. 2019,[14] Eisenberg & Maziak, 2020 suggest exposure to lipids in e-liquids may be a cause[15], Hayeck et al. 2020 suggest a possible interaction between e-liquid solvents (PG and VG) and lung tissue surfactants [16], and Kleinman et al. 2020, suggested nickel alloys as a possible cause.[17] These theories and the supporting early-stage research do not establish nicotine vaping as a cause of EVALI, and the results are open to differing interpretations. More importantly, these theories cannot explain the geographically localised and time-concentrated nature of the EVALI outbreak; why this would coincide exactly with a THC supply chain problem and cause the same symptoms; or how it cleared up without remedial action to address these possible causes in nicotine vaping. This is not to suggest there is no value in the research cited above, it just cannot provide an explanation for the pattern of EVALI lung injuries seen in the United States in 2019.
- There may have been isolated cases outside the United States[18]. These may arise from international travel or internet commerce, but there does not appear to have been a noticeable outbreak in Europe. It is possible that there are occasional cases of acute respiratory distress syndrome or other severe lung injuries that happen to people who use e-cigarettes, without e-cigarettes being the cause. It is also possible that vaping might trigger a severe adverse reaction in someone with an underlying vulnerability, allergy, or pre-existing condition. But this would be manifest in a scattering of cases that would not have a particular geographic or temporal concentration. There is no compelling evidence that this is a material problem with nicotine vaping. If there was such evidence, it would be nothing to do with the EVALI outbreak, which, as discussed above, can be explained convincingly and completely as a problem arising from sales of illicit THC vaping products containing oils that were cut with Vitamin E Acetate.
Implications
- Commentators should stop claiming that nicotine vaping is implicated in “EVALI”. Agencies, academics, journals, peer reviewers, health organisations, activist groups, foundations, media commentators, and politicians should stop falsely asserting or implying that nicotine vaping was or is a cause of EVALI. It is ethically inappropriate to use false or tenuous claims or exaggerated doubt about risks to try to change the behaviour of others. That ethical problem is compounded in this case, because of the risk that users would be deterred from switching from high-risk to low-risk nicotine products and would therefore suffer harm on the basis of unreliable public health information.
- “EVALI” should be renamed to reflect the real risks. The contrived naming of this condition as “E-cigarette, or Vaping, product use-Associated Lung Injury” (EVALI) is misleading and the language is unnecessarily vague. Users and suppliers of THC vapes do not generally use the term “e-cigarettes” to describe THC vaping products such as vape pens. The term “e-cigarette” is primarily used to refer to nicotine vaping products,[19] and the term EVALI, by implicating e-cigarettes, is therefore misleading to nicotine users. At the same time, THC users are misled by an overly broad definition that seems to include all possible vaping products. But it is clear that the 2019 lung injury outbreak was attributable to a specific cause: Vitamin E Acetate added to THC oils for vaping. As one researcher who has called for renaming EVALI puts it, we would not describe the “opioid epidemic” as the “analgesic epidemic”.[20] Others should define the best terminology to accurately communicate the nature of the risk to right target audiences. However, given it coined the phrase, CDC should take responsibility for changing what has become misleading terminology that was introduced when less was known about the lung injury outbreak.
- Risk communicators should address the residual false risk perceptions. The false risk perceptions created during the crisis period in 2019 persist today, yet the causes are now clear and the episode is, for all practical purposes, over and unlikely to recur in the same form. Without action to address residual risk misperceptions, there is a danger that this episode will go down as a public health failure, in which nicotine vapers were needlessly frightened away from a beneficial behaviour change, while THC users were given inadequately precise risk information.[21] There needs to be a concerted effort to put the record straight and to stop unfounded doubt that is negatively affecting risk perceptions and health behaviours. Journals and authors should review academic papers that refer to EVALI and correct or qualify false or misleading statements. Health organisations, including the World Health Organisation, should review their public health communications and advice to practitioners. Advocacy groups and foundations should correct campaign literature and media or political communications.
- EVALI strengthens the case for legalisation and regulation of cannabis products. The lung injury outbreak was caused by the reckless behaviour of actors in an illicit supply chain meeting ongoing demand for cannabis from millions of consumers. Past 30-day cannabis prevalence among US 12th grade students (age 17-18) has been around 20 percent for 25 years,[22] with 11.8 million young adults reporting cannabis use in the past year (2018 data).[23] This high level of use is despite the cannabis trade being illegal at federal level and at state level throughout the United States for most of that period. Prohibition does not prevent access to these products, it changes how such products are made available and who supplies them. Compared to prohibition, the EVALI outbreak suggests it would be better for public health to have regulatory regime that permitted cannabis products to be made available with acceptable safety standards while minimising risks from rogue producers. Such a regime could require listing of ingredients, listing of psychoactive active ingredients at known strengths, appropriate warnings, and restrictions on retail availability, marketing and branding. European Union regulation bans the use of vitamins in nicotine vaping products[24], though primarily to limit appeal rather than for safety reasons. This may have given some reassurance to nicotine vapers in the EU accessing legal nicotine products,[25] but it would not stop rogue THC vape products being made available illicitly and without any regulatory supervision. Cannabis legalisation is a multi-faceted issue and cannot be justified or rejected just on the basis of the experience with EVALI. However, the experience of EVALI provides an additional argument in favour of legalisation and regulation of cannabis products.
Feedback and review
The author would welcome feedback and critical and constructive review of this analysis.
References
- a, b, cU.S. Centers For Disease Control and Prevention (CDC). (2020). Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products.
- ^Coral Gartner, Billie Bonevski, Wayne Hall. (2020). Miscommunication about the causes of the US outbreak of lung diseases in vapers by public health authorities and the media. Drug Alcohol Rev., vol. 39 (1), 3-6. doi:10.1111/dar.13024.
- ^Wayne Hall, Coral Gartner, Billie Bonevski. (2020). Lessons from the public health responses to the US outbreak of vaping‐related lung injury. Addiction, vol. 116 (5), 985-993. doi:10.1111/add.15108.
- ^Dhaval Dave, Daniel Dench, Donald Kenkel, Alan Mathios, et al. (2020). News that takes your breath away: risk perceptions during an outbreak of vaping-related lung injuries. J Risk Uncertain, vol. 60 (3), 281-307. doi:10.1007/s11166-020-09329-2.
- ^Harry Tattan-Birch, Jamie Brown, Lion Shahab, Sarah E Jackson. (2020). Association of the US Outbreak of Vaping-Associated Lung Injury With Perceived Harm of e-Cigarettes Compared With Cigarettes. JAMA Netw Open, vol. 3 (6), e206981. doi:10.1001/jamanetworkopen.2020.6981.
- ^Action on Smoking and Health (UK) & YouGov. (2021). Use of e-cigarettes among adults in Great Britain, 2021.
- ^Kate Kelland. (14 October 2019). Vaping illness, deaths likely very rare beyond U.S., experts say. Reuters.
- ^Benjamin C. Blount, Mateusz P. Karwowski, Peter G. Shields, Maria Morel-Espinosa, et al. (2020). Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI. N Engl J Med, vol. 382 (8), 697-705. doi:10.1056/nejmoa1916433.
- ^U.S. Centers for Disease Control and Prevention. (20 December 2019). Transcript of December 20, 2019, Telebriefing: Update on Lung Injury Associated with E-cigarette Use, or Vaping.
- ^David Downs. (30 August 2019). Vape pen lung disease has insiders eyeing misuse of new additives. Leafly.
- ^David Downs. (10 January 2020). Vape pen lung injury: Here’s what you need to know. Leafly.
- ^Shannon Kozlovich,; Arit M Harvanko; Neal L Benowitz. (2021). Vitamin E Acetate is not Soluble in Nicotine E-liquids. Tobacco Regulatory Science, vol. 7(2) pp 130-134 .
- ^Angelo LeVito. (20 November 2019). Doctors treating deadly lung disease face a problem: Some patients lie about vaping. CNBC (news website).
- ^Matthew C. Madison, Cameron T. Landers, Bon-Hee Gu, Cheng-Yen Chang, et al. (2019). Electronic cigarettes disrupt lung lipid homeostasis and innate immunity independent of nicotine. doi:10.1172/jci128531.
- ^Thomas Eissenberg, Wasim Maziak. (2020). Are Electronic Cigarette Users at Risk for Lipid-mediated Lung Injury?. Am J Respir Crit Care Med, vol. 201 (8), 1012-1013. doi:10.1164/rccm.201910-2082le.
- ^Nathalie Hayeck, Carl Zoghzoghi, Ebrahim Karam, Rola Salman, et al. (2021). Carrier Solvents of Electronic Nicotine Delivery Systems Alter Pulmonary Surfactant. Chem. Res. Toxicol., vol. 34 (6), 1572-1577. doi:10.1021/acs.chemrestox.0c00528.
- ^Michael T. Kleinman, Rebecca Johnson Arechavala, David Herman, Jianru Shi, et al. (2020). E‐cigarette or Vaping Product Use–Associated Lung Injury Produced in an Animal Model From Electronic Cigarette Vapor Exposure Without Tetrahydrocannabinol or Vitamin E Oil. JAHA, vol. 9 (18). doi:10.1161/jaha.120.017368.
- ^Ruth Elizabeth Evans, Sophie Herbert, William Owen, Deepak Rao. (2021). Case of e-cigarette or vaping product use-associated lung injury (EVALI) in London, UK. BMJ Case Rep, vol. 14 (4), e240700. doi:10.1136/bcr-2020-240700.
- ^Robert West. (2019). E-cigarette. doi:10.32388/484818.
- ^Jonathan Foulds. (7 December 2020). Lets call EVALI what it is: THC VALI (rapid response to BMJ case report: Vaping-induced lung injury in a 21-year-old woman). BMJ.
- ^Clive Bates. (13 April 2020). US vaping lung injury outbreak was a public health fiasco or worse – comment to FDA. Counterfactual.
- ^Richard A. Miech (Principal Investigator). (15 December 2020). Trends in 30-Day Prevalence of Use of Various Drugs in Grades 8, 10, and 12, 1991-2020 (Table 3). Monitoring the Future. University of Michigan.
- ^U.S. National Institute on Drug Abuse. (July 2020). Marijuana Research Report What is the scope of marijuana use in the United States?.
- ^European Union. (3 April 2014). Tobacco Products Directive 2014/40/EU Article 7(6)(a).
- ^John Newton. (29 October 2019). Vaping and lung disease in the US: PHE’s advice. Health Matters. Public Health England.