A new study has found that switching from smoking to vaping can restore the lungs’ primary defence against harmful substances.
This decreases the risk of infection and lung diseases such as COPD and can help to improve symptoms of pre-existing lung diseases.
The study, conducted by a team led by Professor Polosa of the University of Catania, looked at the impact of switching to vaping on a mechanism called mucociliary clearance (MCC).
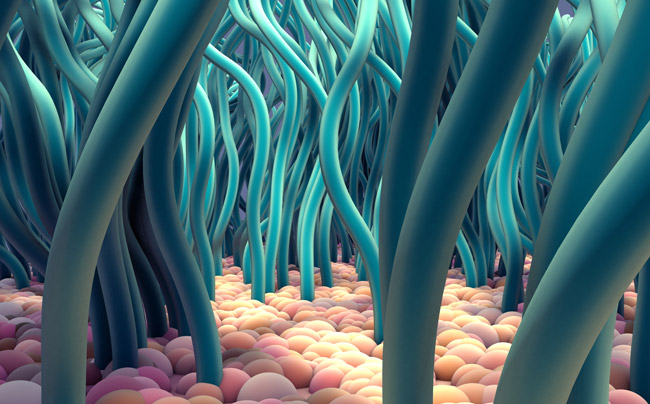
MCC is the process through which tiny hairlike structures on our lungs, called cilia, work like an escalator using mucus to trap and move harmful substances out of our body.
Cigarette smoke contains chemicals that are toxic to cilia and increase mucus production. The damage to cilia means that smokers’ bodies find it harder to remove those harmful substances.
However, Polosa found that people who had switched to vaping or Heat Not Burn (HNB) showed MCC efficiency similar to that of a non-smoker, completely restoring the body’s first line of defence against harmful substances.
This means smokers who have switched from cigarettes regain an important protection against lung infections and inflammation. The improvement in MCC may also protect against development of lung diseases and help to slow down the progression of existing lung diseases.
“This is a remarkable demonstration of complete reversal of damage to the airways,” said Professor Polosa as part of a wide ranging interview with the Ashtray Blog.

The study also suggests a possible reason why some new vapers cough.
Smoking causes excess mucus to build up in the body. However, as the cilia starts to work more efficiently it causes a “functional/purposeful” cough that can last for two to three weeks until the body finally gets rid of excess mucus.
Of course, vaping still carries some risk, even if it is small in comparison to smoking. Polosa explained that small changes in how people vape, such as regularly changing coils, can reduce that risk.
He also explained how science has improved vaping over the last ten years, and how it can further improve it in the future:
“I remember in 2009, when the first reviewed testing from CDC and FDA regarding a bunch of products came out, and at that time there were some constituents of concern.
“However, over the following 3-5 years we witnessed a phenomenal improvement in the overall toxicology of these products. I bet in the next ten years the safety of these products will be enhanced even more.”
Full Interview
What is mucociliary clearance (MCC) efficiency, and what does it mean for health, especially respiratory health?
MCC is the primary defence mechanism of the lungs. Essentially it works as an escalator that moves away noxious stimuli entering the lung when breathing. The functional components of this efficient first line defence mechanism are the protective mucous layer, the airway surface liquid layer, and the cilia on the surface of ciliated cells of the airways.
The MCC defence system is designed to stop viral and bacterial pathogens, particulate matters and gaseous material entering the respiratory system when breathing. In general, airborne noxious stimuli become trapped in the layer of the upper airways (and larger branches of the tracheobronchial tree), and are then subsequently expelled by the coordinated beating of the cilia that propels pathogens and inhaled particles trapped in the mucous layer out of the airways.
In health, this clearance mechanism is effective and protects us from lung infection and inflammatory damage of the airways. But in patients with congenital cilia defects, MCC is highly defective and leads to chronic lung disease. Regular smokers and patients with COPD also show defective MCC indicating structural damage and functional impairment of the respiratory tract.
From a clinical standpoint, dysfunctional MCC may play a role in increased susceptibility of respiratory infections and development of inflammation and obstruction of the lower airways.
Hence, improving MCC is a good thing indicating restoration of one of the most important defence mechanisms of the lung with reduced risk of progression into chronic lung disease.
You also mention the harm to cilia and cilia beating in your study? Can you explain what cilia beating is, and what its importance is?
Healthy cilia are capable of a specific form of coordinated beating that propels pathogens and inhaled particles trapped in the mucous layer out of the airways. They keep the respiratory system clean, sterile and healthy. Regular smoking markedly reduces the efficiency of the MCC defense system.
How? Chronic exposure to harmful chemical constituents in cigarette smoke can cause progressive structural damage and functional alterations of the airway cilia (loss of cilia, chaotic ciliary beating) and excessive mucus secretion. The escalators slow down and become inefficient at clearing pathogens and inhaled particles from the lung.
What is saccharin test transit time (STTT)?
The saccharin test is a non-invasive, well tolerated and simple to perform method that measures the transit time of MCC. In brief, the test consists in measuring the time that takes for an individual to perceive the “sweet taste” of saccharin after placing a saccharin tablet in the nose.
When the sweet taste is perceived the stopwatch is stopped and the recorded time reflects the overall level of efficiency of the MCC. In healthy people (never-smokers), it takes less than 10 min to perceive the “sweet taste” after placing a saccharin tablet in the nose.
How does tobacco smoking affect MCC and STTT, and what does that mean for smokers?
Chronic exposure to harmful chemical constituents in cigarette smoke have been shown to be toxic to cilia and to increase mucus quantity and density. By disrupting the functional components of MCC, smoking contributes to disrupted MCC and lengthened STTT; on average STTT was nearly twice as long in current smokers compared to never and former smokers. MCC restoration is possible in those who quit smoking. In turn, this may reduce the risk of progression to chronic lung disease.
Your study shows that STTT for former smokers who switched to vaping or Heat Not Burn (HNB) was similar to that of non-smokers. How significant is this finding and what implications does it have from a health perspective?
Yes, smokers who switched to exclusive regular use of combustion-free nicotine delivery systems (i.e. electronic cigarettes and heated tobacco products (HTPs)) exhibit exactly similar STTT as never and former smokers. This indicates complete restoration of MCC efficiency!
This is a significant finding, but it is not unexpected. Under normal conditions of use, the level of cilia-toxic chemicals in EC and HTP aerosol emissions are 80-99% lower compared to cigarette smoke. Accordingly, exposure to aerosols generated from combustion-free nicotine delivery technologies is expected to have much less disruptive impact on the functional elements and self-repair characteristics of MCC.
These findings may suggest that combustion-free nicotine delivery technologies are unlikely to have adverse effects on MCC function and add to the evidence that these products do not appear to pose a significant respiratory health hazard.
Is this also connected to why vapers often find their sense of smell and taste improves?
This is probably correct. Chronic inhalation of cigarette smoke may influence not only nasal MCC, but also olfactory function by reducing the number and efficiency of olfactory cells. Careful evaluation of olfactory functions in switching studies of combustion-free nicotine delivery technologies is currently in progress at the Centre of Excellence for the Acceleration of Harm Reduction (CoEHAR) of the University of Catania. Stay tuned!
In the original study you stated that vapers had a lower STTT time (7 minutes) than non-smokers or HNB users. Is this too small to be significant, or were you surprised by this result?
The difference (of about 1 min) observed in the study is too small (and within the variability of the test) to be of any significance. A properly designed prospective switching study of adequate sample size is needed to allow meaningful comparisons.
Can smokers get any benefit if they partially switch to vaping and, in the process, significantly reduce the amount they smoke?
Yes, but only if reduction is significant. The question is: what is a significant reduction in cigarette consumption? There is no perfect answer to this question, but it is important to consider that dual usage cannot be considered a dichotomic behaviour. It is in fact a spectrum depending on the extent of reduction in daily cigarettes. A dual user of 1 or 2 cigarettes a day cannot be equated to a dual user of 12 cigarettes a day, mainly because of compensatory smoking that nullifies any health advantage.
However, smokers massively reducing their smoking from 20 cigarettes to 2 or 3 a day will gain some health advantage. This observation has been demonstrated in studies we have conducted in patients with asthma and COPD.
Some former smokers who are using reduced harm products may be concerned by the potential that they are still breathing in some harmful aerosol emissions. Can vapers make any changes to how they vape/what they use to reduce aerosol emissions?
Yes, for example by regularly changing the coil, you are going to substantially reduce the amount of carbonyls and other toxicants in the aerosol generated under suboptimal conditions of use.
One thing I advise sometimes is to use Mouth-to-Lung devices instead of Direct-Lung devices.
That makes great sense! If you direct-lung inhale, you will introduce a larger amount of aerosol into your lungs. Even if the toxicological risks of vaping devices are small, those risks can be multiplied by Direct-Lung inhalation, and then a small risk may become significant.
Is there a link between poor MCC and cancer?
Not really. Smoking is the common denominator for both poor MCC and cancer. Smoking is known to be linked to cancer and smoking is also a cause for poor MCC.
Is the improvement in MCC function also linked to why new vapers cough?
Yes, this is a very likely possibility.
Cough is a natural defense mechanism that – besides protecting from inhaling foreign bodies into the bronchial tree – helps clear excessive bronchial secretions. The average person produces about 1 liter of mucus each day, which is propelled upwards by the cilia and constantly swallowed. Cough is triggered in case of excessive production (as when smoking). The more the mucus moves, the more the stimulation of the cough, and the more you cough the more mucus you get rid of. For example, the characteristic smoker’s morning cough helps clear the excess mucus that has accumulated in the smoker’s airways during the night.
The paradoxical cough that is reported by new vapers when they quit smoking is linked to restoration of MCC. The rapid restoration of cilia beating efficiency that follows after you quit smoking by switching to vaping causes the body to get rid of mucus that has accumulated in the body due to previous history of exposure to tobacco smoke. This in turn will trigger a cough that helps expel mucus and can last for two to three weeks (until all excess mucus is removed).
Is there an opportunity, via toxicology, emissions testing and product improvement, for us to further improve the relative risk of vaping compared to smoking?
Product innovation will further reduce the relative risk of vaping compared to smoking. And probably with time current potential concern on the absolute risk of vaping products will be completely resolved with the creation of superior and much safer new generation products.
I remember in 2009, when the first reviewed testing from CDC and FDA regarding a bunch of products came out and at that time there were some constituents of concern. However, over the following next 3-5 years we witnessed a phenomenal improvement in the overall toxicology of these products. I bet in the next ten years the safety of these products will be enhanced even more.
People concerned about the toxicology profile of vaping products, seem not to consider that these technologies are evolving at a fast rate with substantial improvements in terms of overall quality and safety. This has never been possible with tobacco cigarettes; their toxicological profile has been more or less the same since their creation.
Is that something you would like to see regulators bring in?
Yes, but you need to take it one step at a time. Look at the EU standards regulating toxic emission from diesel engines, for example. When the standard was first introduced in the early nineties (then named as Euro 1), the level of reduction of toxic emission was a joke if compared to those of the current regulations (the Euro 6) introduced in 2014. This should not surprise us and mainly for two reasons.
One, limited knowledge and concern about toxic emission in the early stages. Two, introduction of stringent standards could have destroyed the whole automobile industry at once. So you need progressive, incremental testing over time, in order to improve the quality of products and to digest the massive amount of information we are getting from toxicological assessment. And also in terms of risk assessment.
For example, the Tobacco Products Directive 2 is fairly straightforward. The standards for quality and safety of vaping products emission will consider only assessment of nicotine, carbonyls and metals. Nothing else. In future, the next directive should better define toxicological threshold for carbonyls and metals, and consider if flavours should be analysed.
For example, we know that certain flavours can kill cells in-vitro at high concentrations (say, above 20%). However, the same flavours at lower concentrations are relatively harmless to cells – as always it’s the dose that makes the poison. Extensive investigation about safety threshold for different flavours is now needed.
Once again, a big thank you to Professor Polosa for taking the time to explain his study to us.

